 /blog/10-signs-you-need-ozone-therapies-now
/blog/10-signs-you-need-ozone-therapies-now
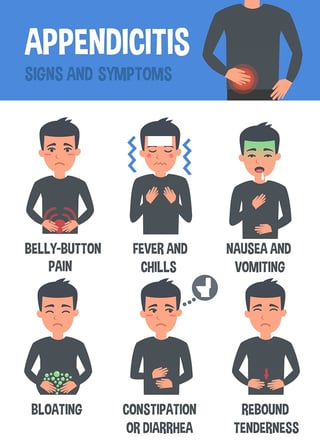
New preoperative testing for appendicitis. Sometimes surgery has to happen.
Four clinical and imaging characteristics can preoperatively identify cases of complicated appendicitis, potentially saving many from long and unnecessary courses of antibiotics.
"In a retrospective study, increasing age and days of pain, combined with the size of the appendix and the presence of an appendicolith on imaging were significantly associated with a histopathologic diagnosis of complicated appendicitis, Jonathan Imran, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress."
His retrospective study of appendectomy patients also honed in on a core issue: 40% of those intraoperatively categorized as having complicated appendicitis actually didn’t have it.
Their research compared the intraoperative designations of simple and complicated appendicitis with the histopathologic diagnosis. They used new predictors, age, duration of pain (days), appendix diameter on imaging, and presence of an appendicolith on imaging. These are the basis of a preoperative risk assessment being developed.
“We hope that these predictors, in combination with improved intraoperative grading, could be used to achieve a more timely and accurate diagnosis of complicated appendicitis,” Dr. Imran said.
"A lot of patients get tagged as complicated but they really aren’t,” said Dr. Imran, a surgical resident at the University of Texas, Dallas. “This definition then guides clinical assessment and has a profound impact on postoperative antibiotics and length of stay. Despite its common use, intraoperative assessment of complicated appendicitis remains subjective.”On the other hand, the standard of a histopathologic diagnosis isn’t available during surgery to guide postoperative management. Dr. Imran and his colleagues sought to create a risk assessment tool to identify patients at risk of complicated appendicitis on the basis of clinical and imaging findings.
They retrospectively examined 1,066 patients who underwent appendectomy at a single institution from 2011 to 2013. They compared the intraoperative designations of simple and complicated appendicitis with the histopathologic diagnosis.
Of the 827 patients designated as having simple appendicitis during surgery, 763 (93%) were confirmed by histopathology. The remainder had complicated appendicitis on histopathology.
Of the 239 patients designated as having complicated appendicitis during surgery, 143 (60%) were confirmed by histopathology. The remainder actually had simple appendicitis. Of these 96 patients, 60% went on to have prolonged courses of antibiotics that, by definition, were unnecessary.
The team then looked at 30 patient variables in an attempt to construct a prediction tool. Among the significant associations with a complicated presentation were older age, type 2 diabetes, longer duration of pain, less lower left quadrant pain, higher median temperature, higher serum creatinine, longer time from presentation of symptoms to surgery, larger appendix diameter, abscess, and the presence of an appendicolith.
Four of these factors remained significantly associated with complicated appendicitis in a multivariate regression analysis:
• Age (per 10 years) – odds ratio, 1.25.
• Duration of pain (per day) – OR, 1.21.
• Appendix diameter on imaging (per mm) – OR, 1.10.
• Presence of an appendicolith on imaging – OR, 1.65.
These findings are the basis of a preoperative risk assessment score the team is developing, which will be prospectively tested.
/blog/10-signs-you-need-ozone-therapies-now
“We hope that these predictors, in combination with improved intraoperative grading, could be used to achieve a more timely and accurate diagnosis of complicated appendicitis,” Dr. Imran said. This study is groundbreaking because it questions the standard of care and brings new light to evidence-based practice.
'You don't do something just because that is the way we have always done it."
If surgery is not an emergency or you are recovering post-op - you can consider I.V. Ozone therapy with German biologics to bolster your immune system and reduce inflammation. Ozone has been shown to make antibiotic therapy more effective. We have had patients come for I.V. Ozone therapy prior to elective surgery to boost their immune function and lessen the chance of a nosocomial infection picked up from the hospital. It would be great to see ozone integrated into surgery to prevent infection. Until that day arrives, patients can choose I.V. ozone therapy outside the surgical arena. All I.V. therapies are MD ordered.
/blog/10-signs-you-need-ozone-therapies-now
/blog/6-misconceptions-about-ozone-therapies
/blog/ozone-therapy-advanced-treatment-for-chronic-infections-second-nature-care-1


